404 Page Not Found
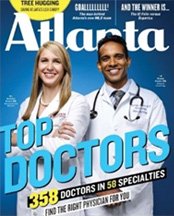
Dr. Chacko Featured on the Cover of
Atlanta's Top Doctor Magazine
We’re sorry, but the page you are looking for may have moved or doesn’t exist. Here are some other resources that may be helpful to you.
Atlanta’s Top Sinus, Asthma and Allergy Doctor
The Chacko Allergy, Asthma and Sinus Center provides Atlanta and the surrounding area with excellent one-on-one care for anyone suffering with any type of asthma, allergy or sinus issue.
Chacko Allergy, Asthma and Sinus Center treats all types of allergies, including the following.
They also provide treatment for many sinus issues, including the following.
- Nasal allergies
- Nasal polyps
- Pediatric ENT treatment
- Postnasal drip
- Sinus headaches
- Sinus infections
- Sinusitis
As part of Chacko Allergy, Asthma and Sinus Center’s allergy treatment, oral immunotherapy treatment can provide relief from even severe cases of food allergies, including peanut allergy.
To read more about the Chacko Allergy, Asthma and Sinus Center and our patients’ success stories, check out our blog. You can also access some of our reviews and learn how Chacko Allergy, Asthma and Sinus Center has helped others successfully manage and treat their allergies, asthma and sinus issues.