Allergies, Asthma and the Hygiene Hypothesis
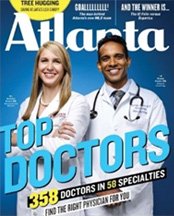
Dr. Chacko Featured on the Cover of
Atlanta's Top Doctor Magazine

Leading medical researchers have offered the “hygiene hypothesis” to explain the rising number of diagnosed allergy and asthma cases. The theory maintains that modern living environments are simply too clean and germ free. Exceptionally clean environments deprive children of the number and types of germs necessary to train a human immune system to recognize the difference between harmful and harmless irritants.
Understanding the Hygiene Hypothesis
Health studies have revealed that people living on farms have fewer allergy related diseases, giving credence to the hygiene hypothesis. Farm animals expose residents to significantly higher levels of endotoxin, a component of germs. Endotoxins decrease allergic inflammation by stimulating immune responses. Research findings also indicate that the development of allergies and asthma may be more complex than the hygiene hypothesis suggests.
Pharmaceutical Medications
Some researchers have suggested that the use of antibiotics, acetaminophen, Tylenol and other drugs may also contribute to the rapid increase in asthma and related diseases. There is a striking parallel between the increased use of antibiotics and the incidence of such diseases. The use of antibiotics during the early years of childhood negatively impact bacterial flora and the disease fighting ability of the immune system.
Lifestyle Factors
Other experts believe that lifestyle choices such as changes in diet and exercise are to blame for the increase of allergies and other chronic diseases. Obesity, in particular, is often cited as a contributing factor to asthma and chronic disease cases. Other researchers have pointed out that the rise in asthma cases may be connected to inadequate levels of vitamin D. It is generally agreed that children aren’t getting a sufficient amount of sunshine to maximize vitamin D levels.
Clean Environments and Disease
Immunobiochemistry scientists are endeavoring to understand the inflammatory mechanisms that underlie the hygiene hypothesis. Making sense of the relationship between respiratory viruses and allergic diseases such as asthma may hold the key. To this end, researchers are investigating the respiratory syncytial virus (RSV), a viral pathogen encountered by most infants. It is well known, for example, that infants who contract RSV pneumonia are more likely to develop childhood asthma. It seems that RSV is associated with a molecule known as the F protein. Interestingly, this particular protein has the ability to flip a vital switch in the immune system.
Under the best of circumstances, humans host a tremendous population of bacteria. These bacteria serve the purpose of educating the immune system of a developing child, allowing the TLR4 switch to be activated. When this bacterial education mechanism is lacking or weak, the link between RSV and the immune infection defense system, known as T-cells, just might initiate the onset of asthma rather than protect the child from infection. Although the exact relationship between bacteria and the human immune system remains a mystery, Researchers seem to be closing in on the answers they desire.
Do You Know What Is Causing Your Allergies?
The Hygiene Hypothesis is an interesting theory. If you want to find out what is causing your allergies and get treatment for them, contact us today. Make an appointment at one of the Chacko Allergy, Asthma and Sinus Center clinic locations in Alpharetta, Atlanta, Canton, Cumming, Druid Hills, Duluth and Johns Creek. Call us at (678) 668–4688.